
Sneeze

Exercise

Laugh

Cough

Walk
then you may suffer from Stress Urinary Incontinence (SUI).
SUI is when urine leaks out during moments of physical activity that increases abdominal pressure, such as coughing, sneezing, laughing, or exercise.
This condition is caused by a weakness of the pelvic floor muscles, which usually tends to happen as we get older, with pregnancy and with certain pelvic floor conditions.
Stress urinary incontinence is the involuntary loss of urine during physical activity, which may include but is not limited to:
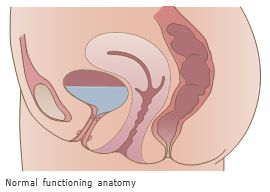
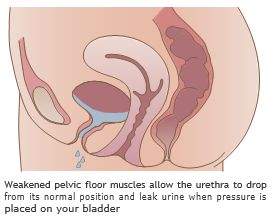
Incontinence occurs when the muscles that support the urethra (the tube that carries urine out of the body) are weakened or damaged. This can happen as a result of childbirth, trauma, hormone changes and many other reasons. You don't have to live like this. This type of incontinence can be treated both surgically or nonsurgically.
One condition is called hypermobility, “hyper” means too much and “mobility” refers to movement, which can result from childbirth, previous pelvic surgery or hormonal changes. Hypermobility occurs when the normal pelvic floor muscles can no longer provide the necessary support to the urethra. This may lead to the urethra dropping when any downward pressure is applied, resulting in involuntary leakage.
Another condition is called intrinsic sphincter deficiency, also sometimes referred to as ISD. This refers to the weakening of the urethral sphincter muscles or closing mechanism. As a result, the sphincter does not function normally regardless of the position of the bladder neck or urethra.
Stress urinary incontinence can be treated in several ways, depending on the exact nature of the incontinence and its severity.
As disease state and anatomy differ for each patient, outcomes may vary. Consult your physician for all available treatment options.
Including traditional mesh slings, single incision mini-slings, retropubic colposuspension and bulking
As with most surgical procedures, there are potential risks and complications associated with this SUI surgery. Your physician can further explain your specific risks based on your medical history and surgical approach used.
You've got questions, and we've got answers!
Stress Urinary Incontinence is the involuntary loss of urine during physical activities, like laughing, jumping, sneezing or lifting heavy objects. It’s the most common form of urinary incontinence.
Stress Urinary Incontinence is the involuntary loss of urine during physical activity, which may include but is not limited to: coughing, laughing or lifting. Incontinence occurs when the muscles that support the urethra (the tube that carries urine out of the body) are weakened or damaged. This can happen as a result of childbirth, trauma, obesity, family history, hormone changes and many other reasons.
One type is called hypermobility, “hyper” means too much and “mobility” refers to movement, which can result from childbirth, previous pelvic surgery or hormonal changes. Hypermobility occurs when the normal pelvic floor muscles can no longer provide the necessary support to the urethra. This may lead to the urethra dropping when any downward pressure is applied, resulting in involuntary leakage. Another type is called intrinsic sphincter deficiency, also sometimes referred to as ISD. This refers to the weakening of the urethral sphincter muscles or closing mechanism. As a result, the sphincter does not function normally regardless of the position of the bladder neck or urethra.
Many times, conservative treatment options for stress urinary incontinence are used initially. Some of those treatment options include behavioral modification — such as decreasing fluid intake, timed voiding and eliminating caffeine, or pelvic floor muscle training such as kegel exercises to strengthen the pelvic floor and sphincter muscles. These types of treatments may or may not improve symptoms. When symptoms are more severe, or conservative options aren’t working, bulking agent injections or surgery may be an option.
Stress urinary incontinence can be treated in several ways, depending on the exact nature of the incontinence and its severity. As disease state and anatomy differ for each patient, outcomes may vary. Consult a specialist for all available treatment options.
A mid-urethral sling system is designed to provide a hammock of support under the urethra to prevent it from dropping during physical activity.
Many surgical options have been developed, the difference being how the mesh material is placed under the urethra. As disease state and anatomy differ for each patient, as well as the type of Stress Urinary Incontinence, consult a specialist for all available treatment options.
This is a decision that should be made by you in consultation with a specialist. You should have the opportunity to discuss with your specialist all of your treatment options, and then which treatment plan is most appropriate for your specific medical situation.
A minimally invasive sling procedure is estimated to take between 30 to 45 minutes; this estimate can vary for many reasons. Your specialist will discuss the type of anesthesia with you, the specific procedure steps, and should answer all your questions. Mid-urethral sling procedures are frequently outpatient procedures, in which case, most patients return home the same day.
As with most surgical procedures, there are potential risks and complications associated with SUI mid-urethral sling surgery. Your specialist can further explain your specific risks based on your medical history and surgical approach used.
There is no surgery for incontinence that has a 100% cure rate, but mid-urethral slings for bladder leakage have been studied since the mid-1990s and have shown to have high success rates of 80-95% at one year follow-up.
Every patient’s recovery experience is unique, and you should consult your specialist as to what he or she expects in your individual case. As with any surgery, it is expected that you feel some soreness but most patients return to normal activity after a short period of time. Please consult with your surgeon on specific activities to avoid during recovery to achieve optimal outcomes. Before you are discharged from the hospital, you may be given a prescription for an antibiotic and/or pain medication to relieve any discomfort you may experience.
You will be instructed on how to care for your incision area. At the discretion of your physician, most patients resume moderate activities within 2 to 4 weeks, with no strenuous activity for up to 6 weeks. Talk with your specialist about post-procedure complications and when to notify him or her of a potential concern.
Most women see results right after the procedure. Talk with your specialist about what you should expect.
Arizona Center for Bladder Health
523 Rose Lane
Wickenburg, AZ 85390
Get Directions